0 Introduction
There is little debate as to the benefit of using orthopaedic shoes (or glue-on shoes)[1] in the treatment of many hoof and leg disorders, and laminitis is no exception. A sizable number of veterinarians even see this as absolutely necessary. Broad consensus amongst veterinarians and many trimmers holds that orthopaedic shoes are essential in restoring a laminitic foot to normal physiological conditions.
In the following, I am not only going to provide evidence that in contrast to the consensus, this is indeed possible on a bare hoof; I would also like to illustrate how orthopaedic shoeing may even make it more difficult to rehabilitate the hoof and prevent damage from laminitis, rather than making it easier.
1 Hoof damage due to laminitis
Laminitis involves disease to the suspensory apparatus with loss of function and injuries sustained characterising the laminitic foot’s condition. Other structures such as the coronary corium, plantar cushion, sole corium or edge of the coffin bone may also be damaged depending on the extent of the laminitic damage.
Depending on the cause and accompanying circumstances, laminitis may lead to slight to highly serious damage to the suspensory apparatus. Slight damage to hooves tend to recover without further treatment, but if they do not, this is almost always due to new laminitis infliction and the continued cause of laminitis. The latter is usually associated with insulin resistance in horses affected. The first bout of laminitis is usually moderate in EMS horses, and some horse owners unfortunately do not take the problem seriously enough for that reason. Continued overfeeding and lack of exercise are usually followed by a second and third bout of laminitis with more permanent damage to the hoof.[2]
In the following, I will be focusing on more pronounced laminitis. Dealing with a seriously damaged laminitic foot has considerable importance compared to slightly damaged hooves with their effective self-healing capabilities. Trimming plays the most crucial role in determining whether or not the injuries due to laminitis can be rehabilitated.
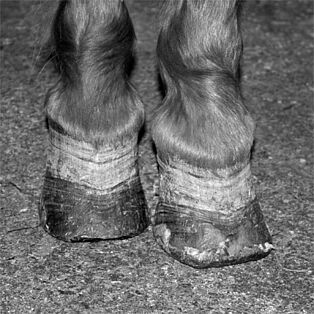
Hooves change at a greater or lesser rate in the months after laminitis where there is massive damage to the suspensory apparatus. The hoof walls, primarily the toe walls, but sometimes also the side walls, take a more oblique angle. The heels vary in height and angle to the ground. The lamellae widen out. These changes are generally regarded as negative, indeed showing deterioration compared to normal physiological condition of the hoof as before laminitis. Even so, it needs to be remembered that the changes in the hoof capsule represent an initial direct reaction to changes in the inside of the hoof. Viewed from this angle, the deformed hoof shape corresponds to the “physiological state” of a laminitic foot.
1.1 The lamellar wedge – beneficial healing process or nuisance?
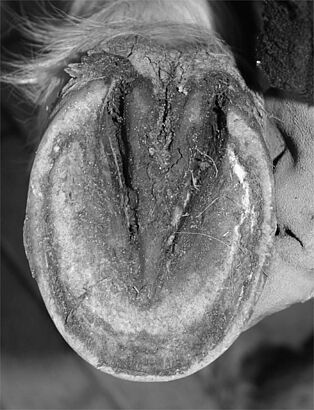
Hoof recovery processes after laminitis usually or even necessarily involve repair to the damaged suspensory apparatus by increased cornification on the lamellar corium. This makes sense, and is often the only way of reaching rapid recovery in the suspensory apparatus. The suspensory apparatus may then differ in structure from the physiologically normal suspensory apparatus, but is highly beneficial in rapidly stabilising the connection between the bone and hoof wall, allowing horses that have overcome acute laminitis to recover fast and get back on their feet.
There is common consensus – which I used to share – that the cornified lamellar wedge keeps the regenerating hoof wall from its normal direction of growth. I have since seen from personal experience (supported and magnified by the experience of my colleagues) that the hoof wall together with the lamellar wedge will reliably find its way to the ground with a little support.
I cannot tell if this will also work if the hoof is left to its own devices. A neglected laminitic foot that has to do without trimming provides no real evidence of the opposite – these horses are usually neglected in other areas such as food and husbandry, so there are always new bouts of laminitis and the remaining deformities in the hooves cannot be taken to be evidence to the contrary. I actually tend more towards the assumption that hooves may well be able to overcome a single bout of laminitis if they have enough of a chance for abrasion and the causes of laminitis have really been resolved. The cornified lamellar wedge grows out and disappears as the hoof capsule regrows as long as the damage only affects the suspensory apparatus. The hoof walls return to their original position relative to the coffin bone, and the laminitic deformities disappear. My assumption arises from my observation of how little trimming I have to do on a laminitic foot as long as soil and husbandry conditions are favourable. All it takes is a little support on my part, and the toe and side walls grow downwards along the front of the coffin bone, pushing the lamellar wedge out within a year.
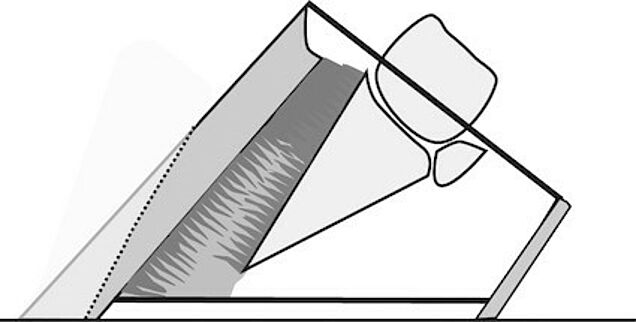
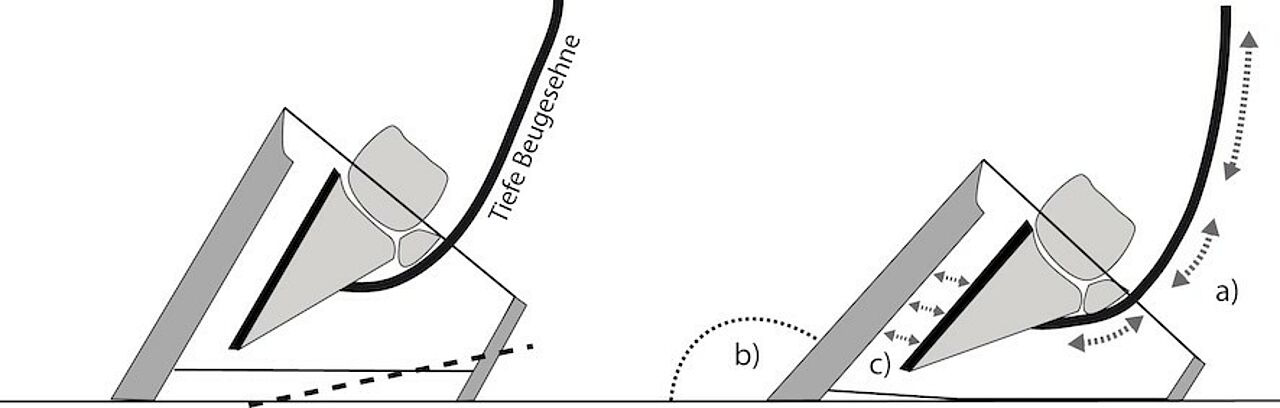
My support mainly consists of thinning and tapered rasping on the toe wall a) to limit its leverage, while b) enabling a certain degree of abrasion, and c) preserving its function as a protective, moisture-retaining wall element needed for stability.
This method is reliable as long as the husbandry conditions for the laminitic horse are ideal,[3]and any existing metabolic issues have been resolved. The lamellar wedge reliably grows out, and the hoof walls grow along the front of the coffin bone restoring parallel alignment between the hoof wall and coffin bone at the end of the process.
Longer durations for the hoof to heal as shown in Fig. 4 usually indicate suboptimal environmental conditions. This is usually feeding that causes laminitis recurrence or slow deterioration, but also persistent, unresolved metabolic problems such as PPID, long-term consequences of cortisone therapy may also prevent the normal healing process in the hooves. The horse in Fig. 2–4 suffered from PPID (Pituitary Pars Intermedia Dysfunction) together with insulin resistance, and unfortunately was allowed out to graze on the paddock.
These impediments hindering laminitis hoof recovery are not rare, unfortunately. However, the principle that the hoof capsule must grow through once again still applies in these cases, even if the process is delayed by minor or even major repetitive manifestations of laminitis damaging the suspensory apparatus.
Regarding the lamellar wedge as a beneficial part of the healing process and accepting the deformed and misaligned walls to the coffin bone as temporary sequelae that will right themselves in time is not generally shared. Most veterinarians and trimmers see the lamellar wedge as nothing but a nuisance, and drastic withdrawal of the toe wall as the best chance of restoring the hoof. The toe wall is often resected as early as in the acute stage of laminitis; the toe is usually also heavily trimmed in the period after laminitis. X-rays often confirm that the toe wall does indeed run parallel to the front of the coffin bone. The only thing is that the toe wall has ceased to exist to a large part, so the alignment can only be claimed without necessarily being true. I see some risks in these procedures that may partly be enough to prevent the hoof’s restoration to health.
1.1.1 Massive toe wall trimming and the consequences on a laminitic foot a) Dehydrated epidermis and damage to the closely connected dermis
Removing the toe wall entails removing the protective layer on the lamellar horn (toe wall resection in the acute stage), or exposes the lamellar wedge that has already formed (restoring alignment, moving the breakover point towards the rear and so on). However, the lamellar horn and wedge formed after laminitis both have poor water-retention capabilities. Removing the hoof wall will leave the horn to dehydrate rapidly.[4]This is serious, considering the direct connection between the cornified lamellae and lamellar horn with the lamellae on the lamellar corium. Sufficient moisture content in the lamellar horn and wedge is vital due to the proximity and direct connection to the soft and fragile lamellae on the lamellar corium. The moisture is only guaranteed as long as the hoof wall covers the lamellar horn and wall, protecting them from dehydration. Under normal conditions, the moisture seeping by diffusion from the living tissues into the adjacent horn will ensure that the cornified lamellae amongst the lamellar corium and also the newly formed lamellar wedge keep a soft and resilient consistency. Removing the hoof wall leads to fast dehydration in the remaining lamellar horn and wedge, which gain a very rigid and brittle consistency.[5]
The lamellar horn and wedge in this condition are not capable of bonding to the fragile lamellae on the lamellar corium without causing pain and injury. I do believe that the harmful effect on the lamellar corium will not only exacerbate the original damage due to laminitis but may actually exceed it. Increased pain may easily follow as is highly noticeable on the bare hoof. Shoeing a hoof treated in this way would reduce the pain again. I do not agree with the frequent conclusion that a laminitic foot will obviously benefit from shoeing with respect to pain – after all, massive trimming on the hoof wall caused the need for shoes or other protection in the first place.
b) Poor hoof stability with consequences for the coronary corium, hoof form and coffin bone rotation angle
Removing the hoof wall around the toe causes deterioration in hoof stability; the toe wall serves not only to protect and retain moisture, but also to provide stability. Removing it causes overloaded side walls and a permanent upward movement of the coronary band on the side walls. The longer this situation lasts, the stronger the curve in the coronary band indicating a move in the coronary corium together with the subcutis below it. This movement cannot be corrected afterwards – that is, even changing the trimming regime back later and leaving the toe wall on the hoof will not give the coronary corium and plantar cushion any reason to return to their old positions. The hoof wall forms on coronary corium, so the shape of the hoof will be permanently altered.
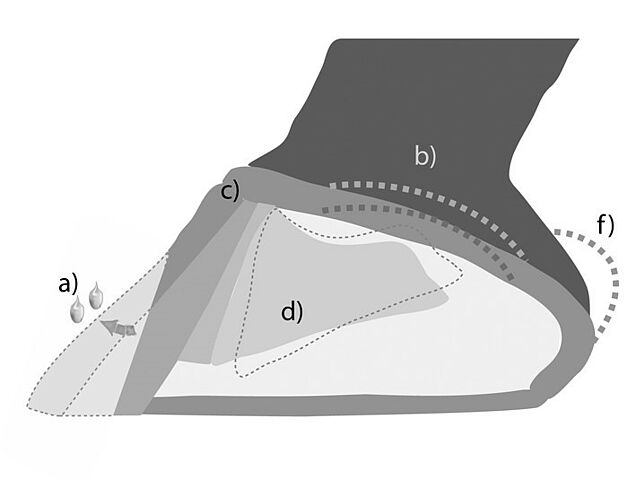
a) Dehydrated lamellar horn and wedge, b) Overload on the side walls and displacement of the coronary region in this area, c) Detrimental effect on positive realignment of coronary corium papillae, d) Potential (further) rotation on the coffin bone, e) Increased sensitivity to pain, f) Raised heels g) Potential side wall rotation
Consider also the comment from my colleague, Astrid Arnold, that a change in hoof stability resulting from removing the toe wall and breaking the wall’s continuity will negatively affect power transfer to the coronary corium. Realigning the papillae on the coronary corium after previous displacement due to a sunk coffin bone and/or toe wall rotation would seem at risk after toe wall resection (Arnold 2017: S. 42 et seq.)
Heavy trimming on the toe wall may cause the coffin bone to rotate (again), posing another potential problem. Two factors can ultimately contribute to this: First, massive trimming on the toe wall often increases pain in the hoof. This increased pain at the base causes increased tension in the flexor muscles, raising tension in the deep flexor tendon and therefore the coffin bone.[6] On the other hand, removing the toe wall weakens deep flexor tendon support. This second factor may also cause the coffin bone to rotate towards the rear.
The additional risk to the suspensory apparatus around the side walls should also be considered. Toe wall removal on a crooked hoof may additionally cause wall rotation as the overload on the side walls always involves additional load on the suspensory apparatus at this position.
1.2 Steepening in the palmar angle of the coffin bone – preventable, recoverable, or acceptable?
Raised heels are a fairly common change to the shape of the laminitic foot. This development is mostly interpreted as the result of more rapid heel growth. However, I do not believe that this is the actual reason for the increase in heel height. The duration of pain can be observed to correlate directly with the increase in the heel height in laminitis patients – that is, the longer a horse remains in its laminitic condition either for systemic reasons or due to incorrect hoof treatment, the greater the tendency towards raised heels. In my view, this is mainly due to pain-related cramping and prolonged tension on the muscles; this ultimately exerts permanent tension on the deep flexor tendon, causing the coffin bone to take a progressively steeper angle.
Can hoof trimming prevent this?
Frequent attempts are made to achieve this. Keeping the thought in mind that “heels grow faster than toes,” trimmers often try to regulate this by shortening the heels. The regrowth on the heels in hooves treated this way can be observed and the heels need to be shortened again at the next appointments in a cycle that is only broken when the pain in the laminitis and hoof subsides and the coffin bone is no longer constantly placed under downward tension. Even so, shortening the heels in what is still a painful situation provides absolutely no guarantee that the above cycle will be broken. On the contrary, there is considerable risk that this will continue the pain, or even cause it to flare up in the first place. Reducing heel height by trimming directly leads to an increase in tension on the deep flexor tendon. The muscular parts of the deep flexor tendon will initially react to this tension by tensing up. Logically, no other second or third reaction will follow later, and the muscles will remain tensed as long as the discomforting tension continues. This will continue until the coffin bone returns back to the palmar angle corresponding to this tensed state with adequate support from the heel. The horse could also possibly find its own “comfortable” heel height by faster heel regrowth, although this is speculation on my part.
At the same time, shortening the heels in this way reinforces the effect of change in hoof angle, tipping the hoof towards the rear and increasing the load on the suspensory apparatus in the toe. This one-sided (repeated) shortening on the rear parts of the hoof will not only increase tension on the deep flexor tendon, but also steepen the toe wall’s angle to the ground, while also additionally increasing the load on the suspensory apparatus in the toe.
The question arises as to whether a raised heel can be restored to its physiological height after the laminitis has healed and the horse and its hooves have recovered.
This is possible in some cases, but not in others. Horses that have contracted a particularly severe bout of laminitis requiring a long time to heal often have higher heels than before. This also always applies to horses with repeated bouts of laminitis preventing complete healing. Ultimately, the high or very high heels are always there and will not return to their normal physiological position if prolonged and/or severe laminitis has left irreparable damage to the coffin bone and corium.
Fig. 11 a-c: This mare suffered repeated laminitis each in successive grazing seasons. She recovered fairly well in between. The heel height corresponds to the painful but still tolerable situation. The coffin bone has sunk, the coffin bone tip and lamellar corium are changed.
Figure 12a-c. This crossbred mare had her first laminitis two years ago due to overfeeding and sudden lack of exercise. This was followed by several relapses, ultimately without full recovery. The heel height corresponds to the position that is always very painful and is currently hardly tolerable for her. The coffin bone tip has sustained serious damage.
The heels will ultimately rise with the pain in the hoof. Accepting this and the height of the heels will be essential for anyone to remember who intends to help the horse by trimming.
Insisting on shortening the heels will not help horses that have returned to a healthy hoof situation after laminitis either. The heel height will diminish the easiest on their own without a trimmer shortening them. This is due to the relationship between pain-related tension and coffin bone angle as mentioned before, and the direct effect of manual heel shortening (see Fig. 10). The easiest and safest path to a flattened palmar angle in the coffin bone and shorter heels is to gradually allow the heel to regain comfort; moderately raised heels will recover on their own with a little support. Support in this case involves disposing of potential obstacles such as high bars, overgrown frog and widened bearing edges at the heel, and generally prevent excessive hoof height or cover.
Soil and husbandry conditions that promote abrasion will help greatly. Since the horse is able to walk quite comfortably again despite still having laminitis hooves at the time of discussion – painlessness is a precondition for the heels to lower again –it will not need hoof protection just to walk or stand, and the necessary abrasion can actually take place. Hoof protection may only be necessary again if the horse is going to resume work on hard and stony soils. I would recommend temporary hoof protection solutions over permanent ones due to the remaining laminitis deformities that still need to be rehabilitated.
2 Why bare hooves?
Even though I initially mentioned in the beginning that a slightly damaged laminitic foot has good self-healing potential, I am not so fanatical about leaving it to nature as to believe that everything would heal itself without any human intervention. I am definitely in favour of humans taking good conscientious care of a pet horse and supporting the horse in whichever way possible in its healing process. The reason I am in favour of bare hoof treatment is not because I think protection is somehow less natural than a bare hoof, but simply because it works well and we have found out the principles as to why it works. These principles cannot apply to a shod hoof (and this applies equally to packing or any permanent protection attached to the hoof) and are therefore unusable.
2.1 Abrasion is good for the laminitic foot
Hoof walls tend to grow too long on any underused hoof, and this also applies to laminitis. A horse with laminitis is initially dependent on rest in the stall until recovery from acute laminitis and sufficient stabilisation in the suspensory apparatus from the lamellar wedge. The horse stands on soft bedding or bandages and is prevented from excessive movement. Once the acute pain subsides, the horse can move more – at least on soft ground, avoiding hard ground at the beginning, but will increasingly be able to take on hard ground with sufficient speed. Even then, abrasion is still only moderate. The range of movement and soil conditions are adapted to the laminitis condition as they should be, and the hooves do not need protection against abrasion. On the contrary, they need any support in new horn being able to abrade. Permanent hoof protection will result in no abrasion whatsoever. This limits the possibility of keeping the hoof in shape for this period; the hoof will be in need of heavy correction at every shoeing, and the trimmer will fall into the predicament of having to correct the hoof when shoeing. Actually, the hoof would even need overcorrection to forestall predictable future development. This is why toe walls are trimmed back very far to prevent excess length again. Heels with a tendency towards raising are heavily trimmed to a greater or lesser extent at each shoeing as well. The consequences of these corrective actions have already been identified, and are effectively inevitable for hooves fitted with protection. Unprotected hooves behave differently, where controlled abrasion ensures that neither the heels nor the toe walls grow too long, instead growing into a favourable shape and position to the ground. The laminitic foot remains in better shape for the period, and strong corrections posing an especially high risk on a laminitic foot are rendered unnecessary.
So in contrast to the prevailing view, I would claim that bare hooves are more easily restored to their normal physiological condition than shod hooves. So far, the consensus has been the reverse with treatment correspondingly at odds in practice:
“Orthopaedic measures in laminitis are aimed at preventing or curbing the risk of coffin bone displacement (STASHAK, 1989b; HÖPPNER, 2004). Orthopaedic shoeing is necessary in incipient coffin bone sinking after the acute symptoms of laminitis have subsided to counteract sinking coffin bones and prevent flaring (RUTHE and MÜLLER, 1997). A corresponding shoe will be especially necessary if the hoof has already deformed.” (Lingens 2008: 39)
Apart from restoring the hoof to its normal physiological condition, laminitis treatment always aims to limit damage and reduce pain. The question arises as to whether these aims are more effectively implemented with a shoe or on a bare hoof.
2.2 Damage limitation and pain reduction
The most effective way of limiting damage is to make sure the existing laminitis subsides as quickly as possible, so all measures necessary and beneficial should be taken to this end. Apart from proper systemic treatment of laminitis,[7] hoof orthopaedics may make an effective contribution by relieving the suspensory apparatus as effectively as possible. Apart from resting in the stall or using a swing lifter to hold or suspend the horse, the most effective ways of achieving this are by redistributing the weight a) from the supporting edge on the sole and frog and b) away from the most heavily affected toes toward the heel part of the hoof. Packing, preferably in a soft and reversibly deformable material, represents a considerable benefit. The packing will need to be individually shaped depending on the hoof’s condition and pain sensitivity on the sole in front of the tip of the frog; bandage fitting is simple and durable. Slightly more packing under the heel often helps lift and improve support to the heel where the hoof-pastern axis is severely flattened or even broken towards the rear. I see raising the heel area as unnecessary or even problematic if the hoof-pastern axis has already steepened or is broken towards the front. Raising the rear part of the hoof may under certain circumstances lead to undesirable load on the suspensory apparatus on the toe wall in these situations, ultimately achieving the opposite of the intended result.[8]
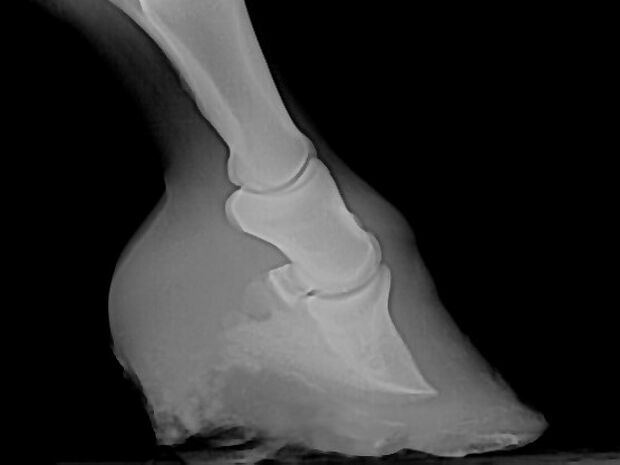
2.2.1 Diagnosis: Coffin bone rotation and following orthopaedic measures
Some horses clinics consider increasing the palmar angle of the coffin bone as a vital initial orthopaedic measure to relieve the suspensory apparatus in laminitis, as is also taught in some university and veterinary college courses. This is based on the assumption that tension on the deep flexor tendon in the acute phase of laminitis will pull the coffin bone towards the rear and out of its original position.[9] X-rays show a gap between the front of the coffin bone and the toe wall as evidence for this assumption. Even dissertations specifically dedicated to this topic[10] and presentation documents fail to distinguish between situations where the coffin bone is in a straight hoof-pastern axis, or has broken out towards the rear. In the first case, hoof wall and coffin bone separation is a result of toe wall movement, and in the second case, the coffin bone may theoretically have rotated towards the rear (coffin bone rotation). There can be no certainty as horses with innate coffin joint flexion are not rare, and are also quite common in horses with laminitis as the “deformity” is not tolerated during trimming (this deformity often only applies to the front hooves), and is constantly corrected by repeatedly shortening the heels.[11]
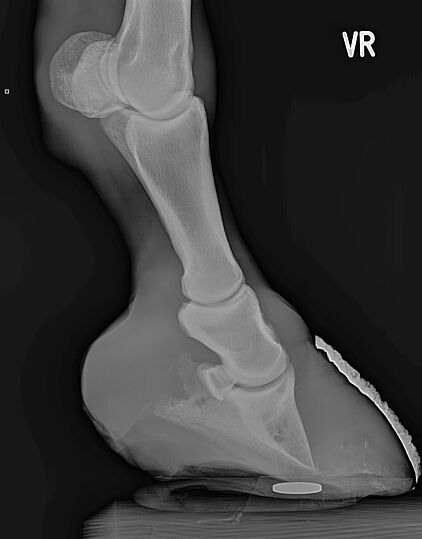
Fig. 14: Five-year-old Morgan mare: This mare has never suffered laminitis, but the x-ray image was interpreted as a certain history of laminitis on pre-purchase examination.
That was not the case. The gap between the bone and the toe wall were solely due to coffin joint flexion as a foal (clubfoot, deep flexor tendon), and years of trying to flatten the hoof angle to match the other limbs.
I would argue that evidence has not yet been rendered for coffin bone rotation during the acute phase of laminitis. One reason is the frequent lack of differentiation in assessing laminitic broadening as coffin bone rotation. Beginning by distinguishing between a continuous and broken hoof-pastern axis as Budras suggests would certainly provide more information to go on.
“The pivot point in coffin bone rotation lies at the coffin joint, and the dorsal toe axis between the coffin bone and the other toe bones appears clearly broken on the x-ray. In contrast, the pivot point in hoof capsule rotation lies in the coronary segment or a few centimetres distal in the dorsal hoof capsule wall. The hoof-pastern axis appears continuous from the side.” (Budras et al. 2008: 19)
Coffin bone rotation late in the chronic phase of laminitis is quite a frequent observation in practice. As I have already stated, I see the main reason for this in the painfully tensed muscles. Pollitt, who also points to a lack of supporting evidence for coffin bone rotation during acute phase of laminitis[12], provides another explanation: that displacement in the terminal and sole edge corium lamellae causes coffin bone rotation in the chronic stage of laminitis, which in turn leads to inwardly directed horn growth.
“Rotation of the distal phalanx is not an acute phenomenon and its appearance does not correlate to when the dorsal hoof lamellae are at their weakest; the acute phase. Instead distal phalanx rotation first appears around six weeks after laminitis development, just when displaced, inward growing terminal wall and sole tubules reach the distal margin of the third phalanx.” (POLLITT 2008: 66)
For these reasons, I see intentionally raising heels to prevent coffin bone rotation in the acute and chronic phases of laminitis as a fight against an imaginary enemy while losing sight of the real problem – the real enemy, if you will. This is hoof capsule rotation as takes place in every case of laminitis, and should be curbed as far as possible.[13] I doubt that raising the heel will help, but I do see it posing a risk of undesirable load on the suspensory apparatus.
Every one of the orthopaedic measures named in limiting damage from laminitis is also used to the same degree to reduce pain. The horse should have the “final word” in all of these measures – whether the horse reacts with an improvement or deterioration in well-being. The horse’s reaction provides an effective insight for trimmers. However, these reactions cannot be understood as a result of a given orthopaedic measure if painkillers have also been administered, as is often the case. I would not recommend withholding necessary drugs from the horse, but I would like to point out that re-administering painkillers followed by an orthopaedic measure does not justify the conclusion that the orthopaedic measure in itself has led to the desired improvement. There is an important distinction.
What are further measures for damage limitation once the acute symptoms of laminitis have subsided?
According to some authors including Lingens, orthopaedic shoeing should always be applied “to counteract coffin bone sinking and prevent flaring” (Lingens 2008: 39). There are various traditional and modern horseshoe and hardware modification types used for this purpose. Additional orthopaedic measures include treatment of the toe wall as already mentioned (toe wall resection, heavy rasping to the toe, thinning down the toe wall) or grooving the hoof below the coronary band.
I have already explained why I consider these measures to be orthopaedically unfavourable. I have also shown how, in my view, shoeing does more to hinder than help healing and corresponding damage limitation. The question arises as to pain reduction, and whether or not permanent hoof protection should be used here.
Assuming that the laminitic horse is in rehabilitation after recovery, the horse will usually not need hoof protection if it has the right soil and husbandry conditions (see footnote 2). Permanent hoof protection is only necessary in reducing pain when horse husbandry or occupation demands it – that is, the horse needs to be sent back to work or management reasons require that the horse is kept on unsuitable ground for the hooves requiring rehabilitation. It may be said that this is the reality for some laminitic horses, which would benefit from shoeing. This is undoubtedly true, but it does not change the increased difficulty of rehabilitating the hoof in these conditions.
When is the right time to send laminitic horses back to work?
There is no definitive time point or period after which a laminitic horse can safely be sent back to work. This may be after three months for some horses or after half a year for others.[14] Bare-hoof laminitic horses signalise this time point clearly by becoming increasingly insensitive to hard soils. I would recommend horse owners to start gently on returning the horse to work and keep a close eye on how well the horse is walking. This is somewhat more difficult to assess in horses with shod hooves.
Soft soil should be considered where early movement is an indispensable part of the treatment programme as is the case in overweight horses with equine metabolic syndrome. If walking wider afield is part of the movement programme, temporary hoof protection should be applied if the horse is still sensitive to the paths used.
2.3 Barefoot treatment and irreversible hoof damage
It depends. The points previously mentioned also apply to rehabilitating or just preserving hooves for damage control: Abrasion is good for the hoof, and heavy correction work is not. Barefoot is therefore also beneficial in these cases. However, there are cases where pain reduction is only really possible after shoeing, although these cases are far less common than is generally believed in my opinion, and this would be evident if the mistake of trying to correct a deformed laminitic hoof into a normal physiological hoof were not made so often.
Irreparable changes to the edge of the coffin bone or coronary, lamellar or solear corium on the tip of the coffin bone resulting in permanent change in the direction of growth of the horn structures will cause the hoof to adopt its final form as a laminitic foot. This can differ substantially from a normal physiological hoof, but trimmers cannot do anything but accept the changed hoof condition. Ignoring this on the assumption that the hoof might benefit from shortened heels[15] with an almost straight and less tilted toe wall or a more rearward breakover point approaching normal hoof physiology will usually come at the price of sacrificing comfort for the laminitic horse.
3. Final thoughts
As a hoof orthopaedist, I am often called to see hooves that have long since passed the acute laminitic phase and show clear signs of laminitis. Unfortunately, I repeatedly see hooves that have been treated for laminitis using all of the tricks of the trade but still show serious damage. Comparing hooves that have been well-managed and trimmed from the outset to neglected hooves with untreated laminitis, I unfortunately often cannot see much of a difference in damage to the hoof in either setting. Sometimes the damage to the hoof in the former is even worse, and the chances of restoring the hoof to a normal physiological condition are less. In my opinion, this is due to lack of respect for the laminitic foot and its own self-healing properties while carrying out the necessary correction work. The currently altered condition of the hoof, reaction to regenerated horn to this new situation and the horse’s attempts to compensate are considered undesirable developments, and orthopaedic measures are directed at their immediate removal. In my view, however, this approach makes it more difficult rather than easier, as intended, for hooves to grow out of their laminitic condition.
References
ARNOLD, A. (2017): Individuelle Unterschiede in der Histopathologie der Hufrehe und Konsequenzen für die Praxis am Huf, In: 11. Huftagung der DHG e.V. für Tierärzte und Hufbearbeiter, Leipzig 10./11. Juni 2017, Tagungsband, S. 40-50.
BUCHNER, H.H.F., (2008): Unterstützende Therapie am Huf bei der Hufrehe: Biomechanische Prinzipien und Validierung von orthopädischen Maßnahmen am Huf, In: Internationales Hufrehesymposium vom 11.-13. November 2008 an der FU Berlin, keine Seitenangaben, Berlin.
BUDRAS, K.-D.; HIRSCHBERG, R-; HINTERHOFER, C. (2008): Hufrehe - Strukturelle Grundlagen und Therapie, In: Der Praktische Tierarzt, Suppl. 6, S. 13-21.
CZECH, C. (2006): Die digitale Phlebographie des an Hufrehe erkrankten Pferdes, Diss., Ludwig-Maximilians-Universität München.
DOHNE, W. (1991) Biokinetische Untersuchungen am Huf des Pferdes mittels eines Meßkraftschuhes, Diss., Tierärztliche Hochschule Hannover.
GLÖCKNER, S. (2002): Eine retrospektive Studie über die Hufrehe bei Pferden; dargestellt an den Patienten der Klinik für Pferde, Allgemeine Chirurgie und Radiologie der Freien Universität Berlin aus den Jahren 1976-1995, Berlin, Freie Universität, Diss.
HAMPSON, B. (2017): Foot pathology on feral horses (Australian Brumbies and Hungarian Przewalskis) - caused by traumatic laminitis or hyperinsulinemia? In: 11. Huftagung der DHG e.V. für Tierärzte und Hufbearbeiter, Leipzig 10./11. Juni 2017, Tagungsband, S. 86-88.
HARDEMAn, L.C.; van der MEIJ, B.R.; BACK, W.; van der KOLK, J.H.; WIJNBERG, I.D. (2015): The Use of Electromyography Including Interference Pattern Analysis to Determine Muscle Force of the Deep Digital Flexor Muscle in Case of Equine Laminitis, In: Equine Vet J, vol. 47: 16. doi:10.1111/evj.12486_36
KLUNDER, P. (2000): Physikalische Auswirkung der Trachtenhochstellung am Huf des Pferdes, Diss., Freie Universität Berlin.
LINGENS, I. (2008): Die Entwicklung der Hufpflege und des Hufbeschlags von der Antike bis zur Neuzeit unter besonderer Berücksichtigung des Hufbeschlags bei der Hufrehe, Diss., Freie Universität Berlin.
PATAN, B.; BUDRAS, K.-D. (2003): Segmentspezifitäten am Pferdehuf. Teil 2 – Zusammenhang zwischen Hornstruktur und mechanisch-physikalischen Horneigenschaften in den verschiedenen Hufsegmenten, In: Pferdeheilkunde, Heft 1, S. 177-184, Stuttgart.
PAUL, N. (2017): Der metabolische Hufrehepatient - Verursacht Insulin eine Überproliferation der Hornkapsel?, In: 11. Huftagung der DHG e.V. für Tierärzte und Hufbearbeiter, Leipzig 10./11. Juni 2017, Tagungsband, S. 80-84.
POLLITT, C. C. (2008): Equine Laminitis Current Concepts, RIRDC, Canberra.
RASCH, K. (2010a): Blutegeltherapie bei Hufrehe der Pferde - Ergebnisse einer bundesweiten Studie, In: Zeitschrift für Ganzheitliche Tiermedizin, Nr.1, 24-29.
RASCH, K. (2010b): Diagnose Hufrehe, Stuttgart.
VAN EPS, A. W.; POLLITT, C. C. (2009): Equine laminitis model: Cryotherapy reduces the severity of lesions evaluated seven days after induction with oligofructose, In: Equine Vet J, vol. 41, S.741-746.
Appendix: Bare hoof rehabilitation on moderately and severely damaged laminitic feet – Examples
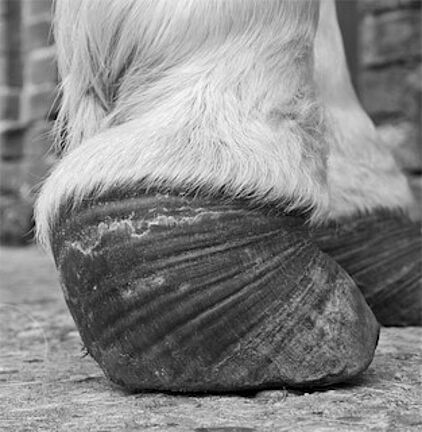
Shire mare, front right: chronic laminitis (both front hooves affected)
Period between before and after images: sixteen months
- This can be considered furthermore, even if not mentioned explicitly.
- And metabolic condition leads to a subclinical “laminitis problem” in these cases, even without explicit laminitis; see Hampson (2017: 86 et seq.) and Paul (2017: 80 et seq.) in this volume.
- Ideal husbandry means keeping the horse with laminitis in sufficiently soft soil conditions in a calm environment without forced movement from other horses or husbandry management. Sandy grounds are optimal and combine well with hard flat surfaces. The latter are mostly well-tolerated if the horse is free to step onto and off them while remaining in step. These surfaces are also highly conducive to the abrasion that a laminitic foot requires to heal and grow back to a healthy state.
- The lamellar horn loses half of its moisture after four to five hours. (Patan; Budras 2003: 180)
- Every trimmer that has ever tried to trim the horn with a rasp or even with a knife knows its rock-hard consistency.
- See also the results from Hardeman et al. 2005
- In my view, these include stall rest, cryotherapy (van Eps; Pollitt (2009), and leech therapy (Rasch 2010a).
- Several studies have used biokinetic measurement to assess the impact of wedges on load distribution on the hoof, but have led to highly contradictory results (Dohne 1991, Klunder 2000, Buchner 2008). In my view, the varying results are due to these studies not taking the respective hoof condition into consideration in the analysis; the situation’s impact on the effect of wedging is substantial, and may explain why different cases yield different results with regard to load distribution and application of force.
- The “artificial” steepening of the coffin bone will always reduce tension on the deep flexor tendon – a “natural” process where the horse gradually adjusts the coffin bone to a steeper angle due to the pain, which is usually not tolerated and corrected by shortening the heel.
- e.g. GLÖCKNER (2002) and CZECH (2006)
- For the context in this type of trimming and laminitis, see RASCH (2010b: p. 62 et seq. and p. 130 et seq.)
- "Palmar rotation of the distal phalanx relative to the dorsal hoof wall was not detected in any radiograph." (VAN EPS; POLLITT 2009: 744)
- An exception lies in hooves that may emerge unscathed from laminitis, which would have to be a slight case.
- Obviously, this also depends on the type of work the horse is expected to perform, and whether the work allows some consideration for hooves that have not yet fully recovered.
- Czech refers to Morrison (2005) in that “all stabilising support structures in the coffin joint, joint capsule, and lateral and sesamoid tendons in long-term chronic laminitic horses are reduced in their flexibility due to fibrous induration” (Czech 2006: 100) – one more reason to keep the heels high, sometimes extremely high.